A corrected claim is a replacement of a previously billed claim that requires a revision to coding, service dates, billed amounts or member information. CORRECTED CLAIM BILLING REQUIREMENTS.What is Corrected Claims A corrected claim is a claim that has already been processed, whether paid or denied, and is resubmitted with additional charges, different procedure or diagnosis codes or any information that would change the way the claim originally processed.
What is corrected claim?
A corrected claim is a replacement of a previously submitted claim. Previously submitted claims that were completely rejected or denied should be sent as a new claim.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
When should you submit a corrected claim?
A corrected claim is appropriate to submit when the provider made an error in the information initially submitted on a claim. is simply creating a new claim and submitting it through your preferred clearinghouse. If you resubmit a claim that has been denied, the new claim will be denied as a duplicate claim.
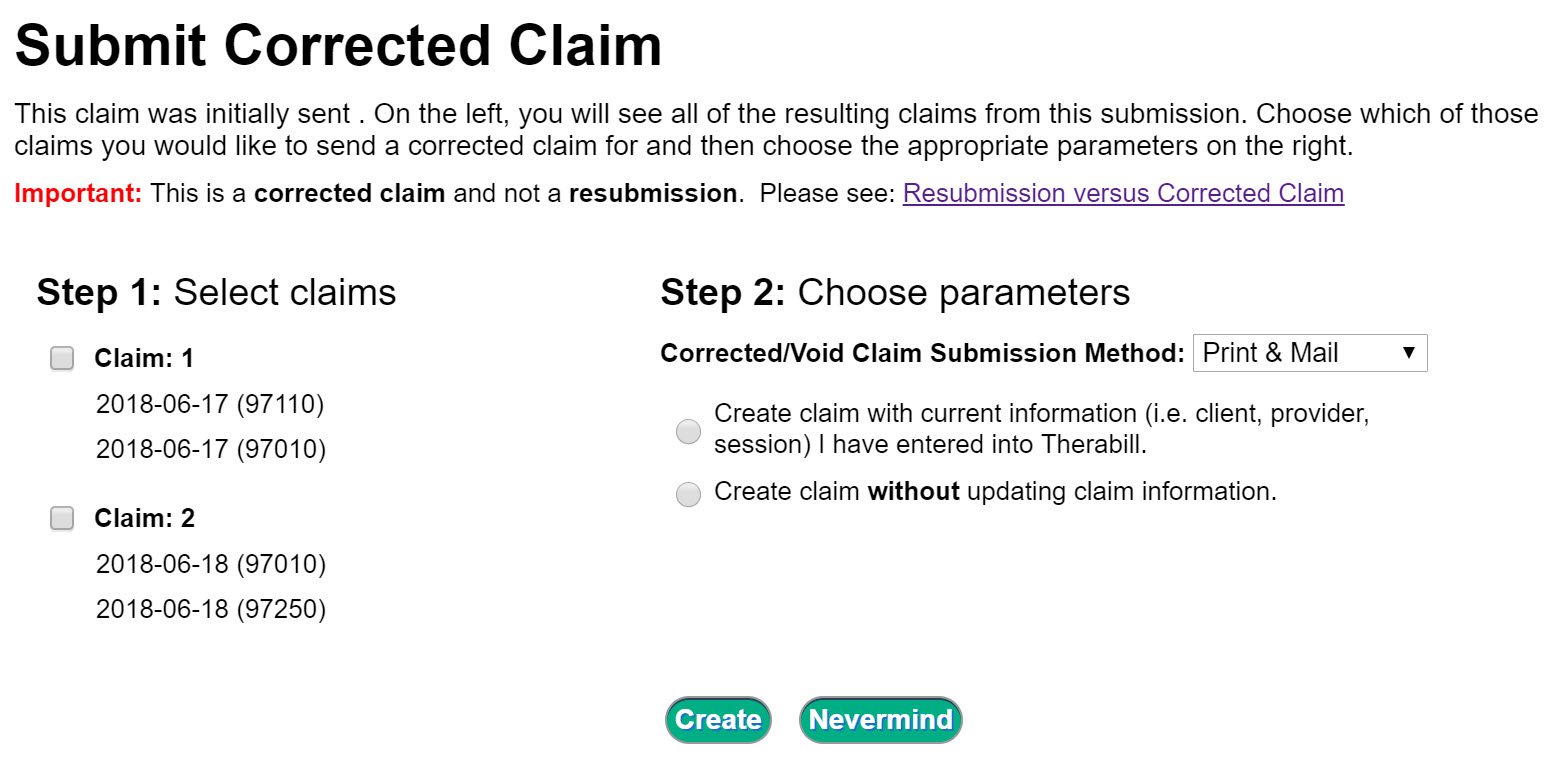
How do I make a corrected claim?
How are Corrected Claims submitted? Claims should be submitted electronically. If a paper claim must be sent, write ‘Corrected Claim’ on top of the claim form and mail to the appropriate claim address on the member’s identification card.
What is corrected claim?
A corrected claim is a replacement of a previously submitted claim. Previously submitted claims that were completely rejected or denied should be sent as a new claim.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
When should you submit a corrected claim?
A corrected claim is appropriate to submit when the provider made an error in the information initially submitted on a claim. is simply creating a new claim and submitting it through your preferred clearinghouse. If you resubmit a claim that has been denied, the new claim will be denied as a duplicate claim.
How do you indicate a corrected claim on 1500?
On the CMS-1500 Form, use Corrected Claim Indicator (Medicaid Resubmission Code). Enter the frequency code “7” in the “Code” field and the original claim number in the “Original Ref No.” field.
Which is considered a voided claim?
Voided Claim: A claim that was originally paid, and then later was canceled and the payment taken back.
What is the resubmission code for a corrected claim?
Complete box 22 (Resubmission Code) to include a 7 (the “Replace” billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.
Does Medicare accept corrected claims?
Therefore, you may submit a new (corrected) claim and it will not reject as a duplicate to the original claim. You must submit a new claim if: You do not have access to the DDE system.
What is the difference between resubmission code 6 and 7?
What is the difference between frequency code 6 and frequency code 7? Frequency code 6 is corrected claim and frequency code 7 is replace submitted claim.
What is an adjustment claim?
Adjustment claims (type of bill XX7) are submitted when it is necessary to change information on a previously processed claim. The change must impact the processing of the original bill or additional bills in order for the adjustment to be performed.
Why is it important that claims be submitted with complete and correct information?
Submitting a claim correctly the first time increases the cash flow to your practice, prevents costly follow-up time by your office or billing staff, and reduces the uncertainty members feel with an unresolved claim.
What is a duplicate claim?
A duplicate claim is a claim a provider is unable to process due to a claim previously submitted for that date of service. NFOCUS considers a Duplicate claim.
How do I fix medical billing errors?
If you get a medical bill that seems incorrect, call the provider and your insurer and explain why the bill seems wrong. Perhaps the doctor simply entered the wrong code or the insurer didn’t receive the bill. If so, ask the provider to resubmit the claim with any necessary corrections.
What is claim resubmission?
For Claims: A “Resubmission” is defined as a claim originally denied because of missing documentation, incorrect coding, etc., which is now being resubmitted with the required information.
Does Medicare accept corrected claims?
Therefore, you may submit a new (corrected) claim and it will not reject as a duplicate to the original claim. You must submit a new claim if: You do not have access to the DDE system.
What is the resubmission code for a corrected claim?
Complete box 22 (Resubmission Code) to include a 7 (the “Replace” billing code) to notify us of a corrected or replacement claim, or insert an 8 (the “Void” billing code) to let us know you are voiding a previously submitted claim.
What is corrected claim?
A corrected claim is a replacement of a previously submitted claim. Previously submitted claims that were completely rejected or denied should be sent as a new claim.
What is the difference between a corrected claim and a replacement claim?
A corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim.
What is a corrected or replacement claim?
corrected or replacement claim is a replacement of a previously submitted claim (e.g., changes or corrections to charges, clinical or procedure codes, dates of service, member information, etc.). The new claim will be considered as a replacement of a previously processed claim. A corrected claim is not an inquiry or appeal.
Should I call the payer or file a corrected claim?
It is always best to call the payer if you are not yet sure how they want claims re-sent. Some payers do not accept Corrected Claims and want corrections sent as a brand new claim. If the payer tells you that you need to file a corrected claim, get the details of how it should be filed. Below is a guideline for how you might approach this.
What does it mean when a claim is incorrect?
This can mean that you are sending them information that was not provided previously or that you think they processed the original claim incorrectly. For more information, please see: Filing a Corrected Claim.
What is a corrected claim bcbsks?
Corrected Claims A request made from a contracting provider to change a claim, (e.g., changing information on the service line, modifier addition, diagnosis correction, etc.) that has previously processed is considered a corrected claim. The submission of a corrected claim must be received by BCBSKS within the 15-month timely filing deadline.